Racial/ethnic disparities during the covid pandemic brought the issue of racism in health and healthcare to the attention of the nation. Some guy I found on YouTube explained it like this (play from 9:09 – 9:57):
The disparities weren’t new, of course. They are centuries old. And people have been studying them for a long time. But for most Americans—White Americans, at least—it was a new realization. Poor health is one of the saddest, most unfortunate results of racialization, and one of the strongest arguments that addressing racialization is a moral imperative.
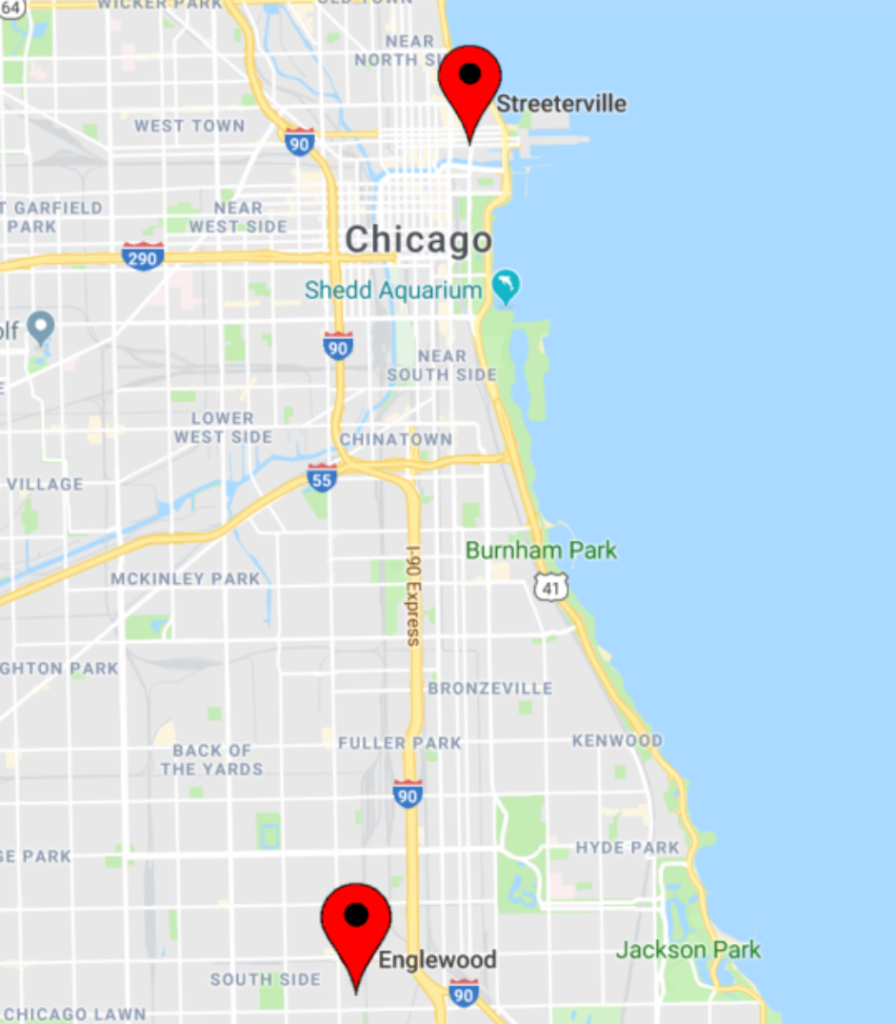
Consider this: Chicagoans who live in Englewood, on the South Side, have a life expectancy of 60 years. Chicagoans who live nine miles north in Streeterville—the Magnificent Mile, Navy Pier—have a life expectancy of 90 years.
Get on the red line at 63rd, go ten stops north to Grand, and increase your life expectancy by 50%—as long as you pick up half a million dollars along the way so you can afford to buy a place to live.
Christina Clarke and her colleagues (2010) found nearly a 20-year gap in life expectancy in California between poor Black men and well-to-do Asian women. They note that this is the same size as the gap between Bangladesh and Japan, and deserves much more attention that we usually give it.
Want to know how long people in your community can expect to live, on average? Enter your address here.
All policies are health policies
If you’re going to understand racial/ethnic disparities in health, you need to understand this first: health is determined primarily by the quality of your life, not the quality of your healthcare. Don’t get me wrong. Healthcare is important. Access to high-quality healthcare is the reason I’m here today, and I am grateful for it. But the U.S. is a perfect example that if you ignore the quality of life for a large proportion of your population, you can spend enormous amounts on healthcare and you’ll still have a whole lot of sick people. Why? The Robert Wood Johnson Foundation explains it like this:
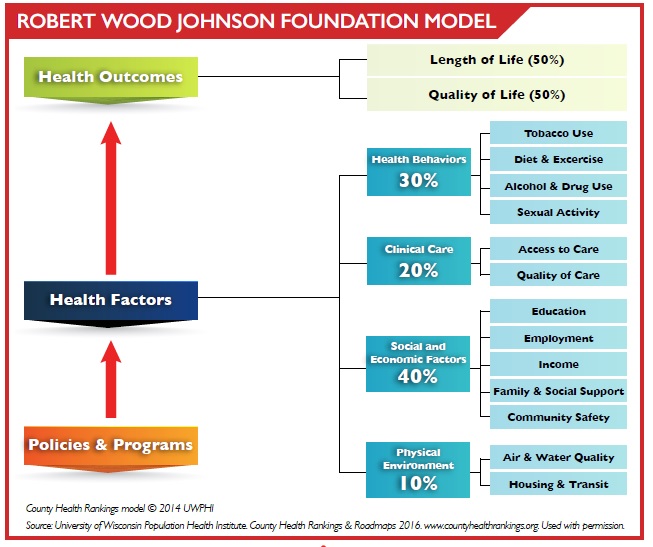
It’s important for all of us, individually, to do everything we can for our health. We have a responsibility to ourselves and to others to be as healthy as we can be. (See the “Health Behaviors” box in the right-hand column.) But that accounts only for about 30% of the variability in health from one person to the next. Access to high-quality health care is also important, but still accounts for only about 20% of the variability in people’s health. The largest single factor, at 40%, is the social/economic context in which we were raised and in which we live as adults. The quality of our physical environment contributes the last 10%.
That’s why, as you can see in the left-hand column, “policies and programs” are the foundation of our health outcomes as individuals and as a nation, both for the length and the quality of our lives. That’s why race/ethnicity and SES are the two best predictors of one’s health in the U.S. Truth is, most of what matters for our health is outside our control.
Here’s something that helped me understand why overall quality of life is more important than health behaviors or healthcare in determing our health. In his excellent book, Health Disparities in the United States, Donald Barr (2019) notes that we tend to assume that new medical treatments lead to improvements in health. Look, for example, at Barr’s chart tracking the decline of tuberculosis in England and Wales in the mid-20th century:
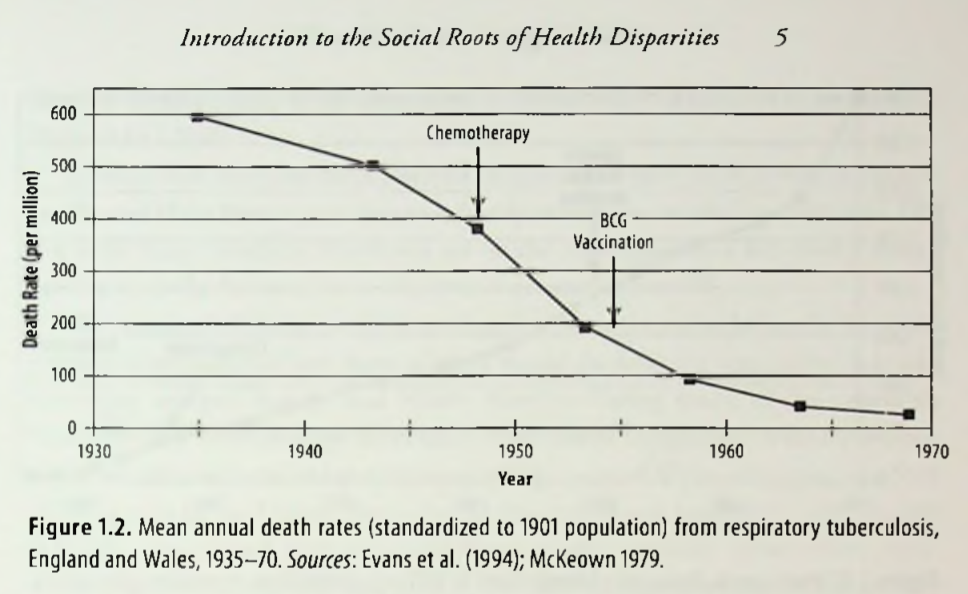
What the chart doesn’t show, however, is that TB started declining in the mid-19th century, long before the cause of the disease was identified, much less the cure:
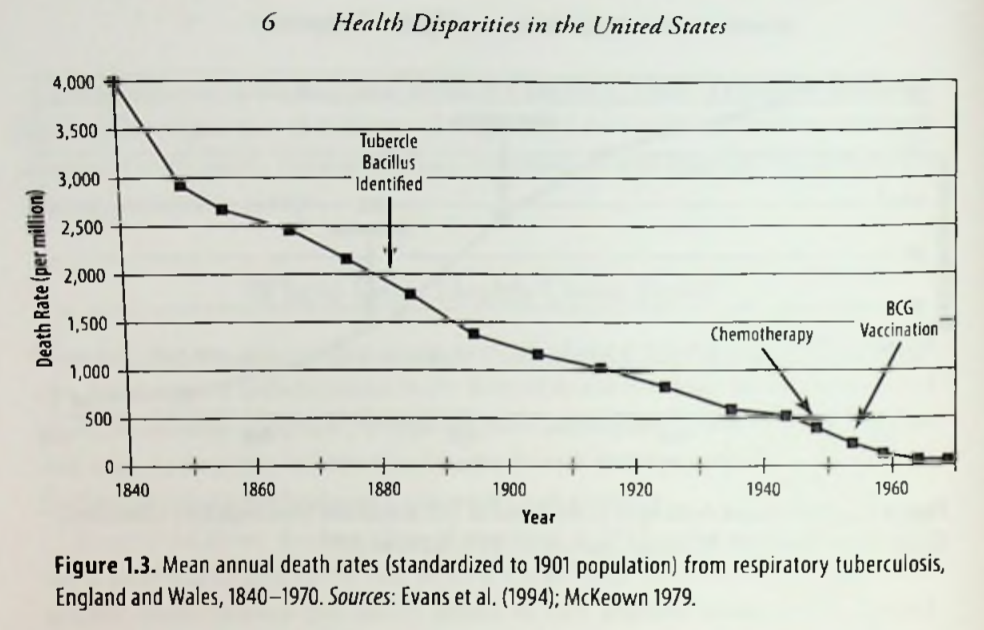
Why? Here is Barr’s explanation:
“[T]he rising standard of living seen in England and Wales in the ninetheenth and twentieth centuries can explain the falling death rates. Better nutrition, better sanitation, better housing, and less crowding, combined with public health measures to prevent the spread of TB, accounted for most of the decline in death rates over the last 200 years.” (Health Disparities in the United States, page 6.)
That’s why all public policy is public health policy. Will we make sure everyone has enough to eat? Will we make sure everyone attends high-quality schools? Will we clean up polluted sites? Will everyone live in a decent home? The answer to each of these questions–and many more–determines the overall, baseline health of the population. If baseline health is low because of poor social and economic conditions, you end up spending trillions of dollars on healthcare—one dollar out of every six, in our case—and you still don’t get good results.
So class matters. I can see that. But why race?
There are three primary answers to that question.
Answer #1: People of color are disproportionately poor
Remember that the racialization of society means that people of color and other marginalized groups have far fewer resources than White people, on average. When class matters, race matters.
Furthermore, not having enough money creates high levels of chronic stress, as well. When stress is both occasional and brief, a strong physiological response is helpful. Think “fight or flight.” But when stress is constant, a strong physiological response is not helpful. In fact, it can result in a great deal of harm. Bruce McEwen was among the first to study the effects of chronic stress, the wear and tear on the body and its organs, which he called “allostatic load.” More colloquially, he referred to it as the difference betweeen being “stressed” and “stressed out.”
Being poor has a negative effect on health objectively and subjectively. And a higher percentage of people of color have to deal with both.
Answer #2: Racism is its own, separate, source of chronic stress
In addition, not being White is a source of stress all its own, regardless of your economic standing. When it comes to health, White people generally fare better than people of color in the same economic class. Poor White people deal with the objective barriers and subjective stress of not having enough money. People of color deal with the objective barriers and subjective stress of not being White. Poor people of color deal with both. A double whammy. A double allostatic load. A double dose of being stressed out. All accompanied by the poorer health that often results.
Courtney Cogburn, a member of the Social Work faculty at Columbia, said this in a Tedx Talk in Richmond, Virginia:
“Our lived experiences contribute to racial inequalities in health. . . For the fifteen leading causes of death . . . Blacks have an earlier onset, faster progression, and earlier death than Whites. . . . even when we account for education, income, and health insurance.”

Arline Geronimus (2006) is a public health researcher at the University of Michigan who has found that Black Americans—of every economic status—age more quickly than White Americans, and the culprit is the chronic stress of racism. On average, Black people are physiologically older than White people of the same age—“weathered,” Geronimus calls it. Naturally, their health is worse as a result. Geronimus says, “Not only do Blacks experience poor health at earlier ages than do Whites, but this deterioration in health accumulates, producing ever-greater racial inequality in health with age through middle adulthood.” In fact, at each decade of life, Geronimus and her colleagues found that nonpoor Black people are at greater risk of a high allostatic load than poor White people. Black women are particularly at risk, whether they were poor or middle class, indicating that they experience greater chronic stress than anyone else in the sample.
This higher allostatic load—not just stressed but stressed out—contributes to the fact that Black people are more likely, among other things, to have high blood pressure, diabetes, and dementia, and are more likely to die from cancer.
Infant health and maternal health are especially poor for African Americans. One reason is that the uterus is a blood-rich organ, and stress damages the uterus in much the same way it damages the heart. Infant mortality, very-low-birthweight babies, and maternal mortality are much higher for Black American women than for White American women—at every level of income and education (Barr, 2019).
Here is an interesting insight into the connection between the stress of racism and the health of pregnant Black mothers: Orchard and Price (2017) measured county-level rates of both implicit and explicit White prejudice against Black people using data from the Implicit Associations Test. They also measured each county’s Black-White gap in the percentage of low-birth-weight babies and in percentage of pre-term births. (Both low-weight babies and early delivery are signs of poor maternal health.) In counties with high implicit racial prejudice, the racial gap in low-birth-weight-babies was 14% higher than in counties with low implicit prejudice; the Black-White gap in preterm births in high implicit prejudice counties was 29% higher. For explicit prejudice, the gaps were even larger: 22% for low-birth-weight babies and 36% for preterm deliveries.
It continues after birth. The American Academy of Pediatrics issued a policy statement (Trent, Dooley, and Dougé, 2019) that concluded that the stress of racism starts early in life, with negative effects on the health of children and adolescents of color. And the cycle continues—Tyan Parker Dominguez and her colleagues (2008) found that racism experienced in their youth predicts Black mothers’ likelihood of giving birth to low-birth-weight babies.
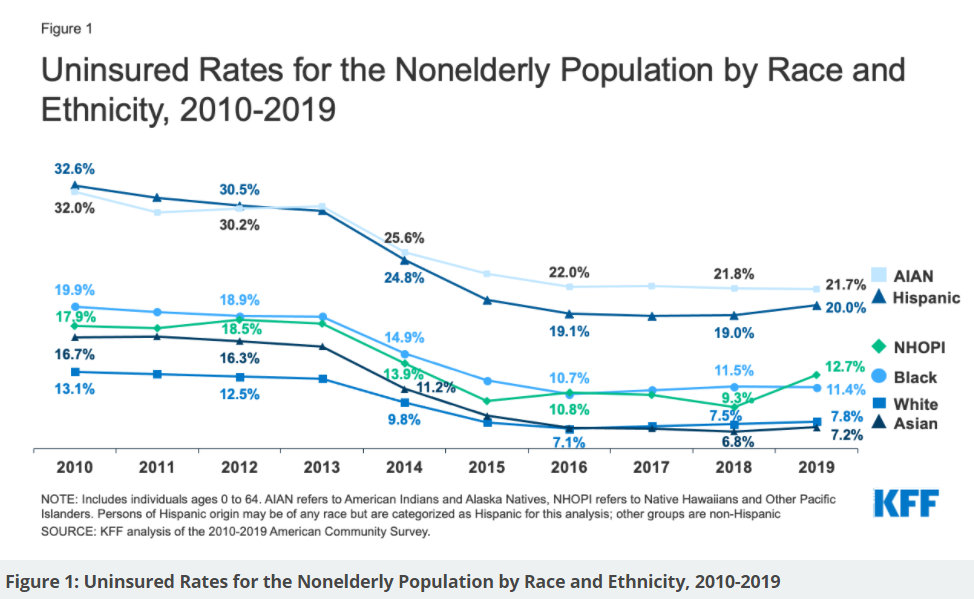
And then there is access to health care, made possible by health insurance. The Affordable Care Act (“Obamacare”) reduced, but did not eliminate, racial/ethnic gaps in healthcare coverage for people under 65. Latinos and Native Americans are the most likely to lack health insurance—approximately 20% of both groups as of 2019. The sickest among us are the least likely to receive care.
Answer #3: People of color get poorer health care—physcial and mental—regardless of economic status
We saw earlier that clinical care accounts for only 20% of the quality of one’s health, but that 20% still matters. Hasnain-Wynia and her colleagues (2010) found that Asian, Black, and Latino patients are more likely to be hospitalized in facilities that score lower, on average, on various measures of quality of care. And that’s a problem of race as well as class.
Unfortunately, just getting to the right hospitial (or clinic, or doctor’s office) isn’t enough for patients of color. Many of them receive worse treatment that White patients even in the best facilities.
Why is that? One big reason is prejudice among healthcare workers, sometimes explicit, often implicit. Penner et al. (2016) reviewed a number of studies of implicit bias on the part of healthcare workers and concluded that, “Non-black (i.e., white, Asian, and Hispanic/Latino) health-care providers display substantial implicit racial bias toward blacks at levels comparable to the general public.”
Not good, obviously, but is it a problem? Yes. Penner and his colleagues say that health-care providers with implicit bias often provide substandard care for their patients of color. In addition, they often don’t interact well with patients of color, either. In their study, non-Black oncologists didn’t spend as much time with Black patients as they did with White patients. Furthermore, neutral observers rated the oncologists as less patient-centered and less supportive overall when interacting with Black patients. The doctors’ poor communication, in turn, left their patients with a poorer understanding of what they had been told and significantly less confidence in the quality of the treatments they were going to receive. Such interactions are even worse when the physician is stressed, harried, or burned out (Dyrbye et al., 2019).
Perhaps that’s why Alsan, Garrick, and Graziani (2019) found that Black male patients are more likely to follow up on recommendations from a doctor (e.g., get a flu shot) when the doctor is also a Black man. The reason? Better communication. Patients opened up more about their concerns and reported that the doctor was more trustworthy. There likely are several reasons for that, but one of them, no doubt, is the absence of implicit or explicit bias, which often leaks out in interracial interactions.
It’s not just bias–sometimes it’s plain old stereotypes. For example, Hoffman et al. (2016) found that half of the White med students in their study believed the old canard that Black people have thicker skin than other people, and feel less pain as a result. They went on to recommend substandard pain treatments for Black patients, something that happens all too often in U.S. healthcare.
What can be done about that? Ivuoma Onyeador and her colleagues (2020) looked at several possibilities and found that the only one that worked was increasing White healthcare providers’ contact with people of color. Educationally-oriented efforts like diversity training didn’t do much, but getting to know people of color as people made a difference. I tell my White pre-health and nursing students: If the only poor people you know are your patients . . . if the only people of color you know are your patients . . . no matter how well-intentioned you may be, you will struggle with implicit bias. We have to be intentional about breaking out of segregated networks if we want to be able to treat everyone fairly. And that goes for teachers, salespeople, ministers, counselors, and anybody else who works closely with other people.
In addition to helping individual providers do their best for all their patients, healthcare systems need to do their best at the organizational level, too. That means asking the right questions and gathering the right information. Here’s one example: In the Journal of the National Medical Association, Cykert et al. (2020) described a five-year effort by Cone Health (a consortium of hospitals in Greensboro, North Carolina) to address the gap between Black and White cancer patients in completing their full round of treatments, roughly 90% for White patients vs. 80% for Black patients). They kept careful track of who was missing appointments and followed up to see why they didn’t make it. Lack of reliable transportation, for example, kept some people from getting all their treatments. By addressing those problems (e.g., by providing rides to those who needed them), Cone Health was able to eliminate their treatment gap, bringing up the number of Black patients who completed treatment nearly to 90%. In healthcare–but also in education, law enforcement, and so many other areas of society—tracking success rates by class and race provides both the motivation and the information necessary for reducing inequities.
It is important to note that health disparities apply to mental health as well as physical health, and for all the same reasons.
Anglin et al. (2021) examined the relationship between systemic racism and the emergence of psychosis in Black and Latino Americans. Their model is useful for understanding a wide variety of health concerns, physical as well as mental:
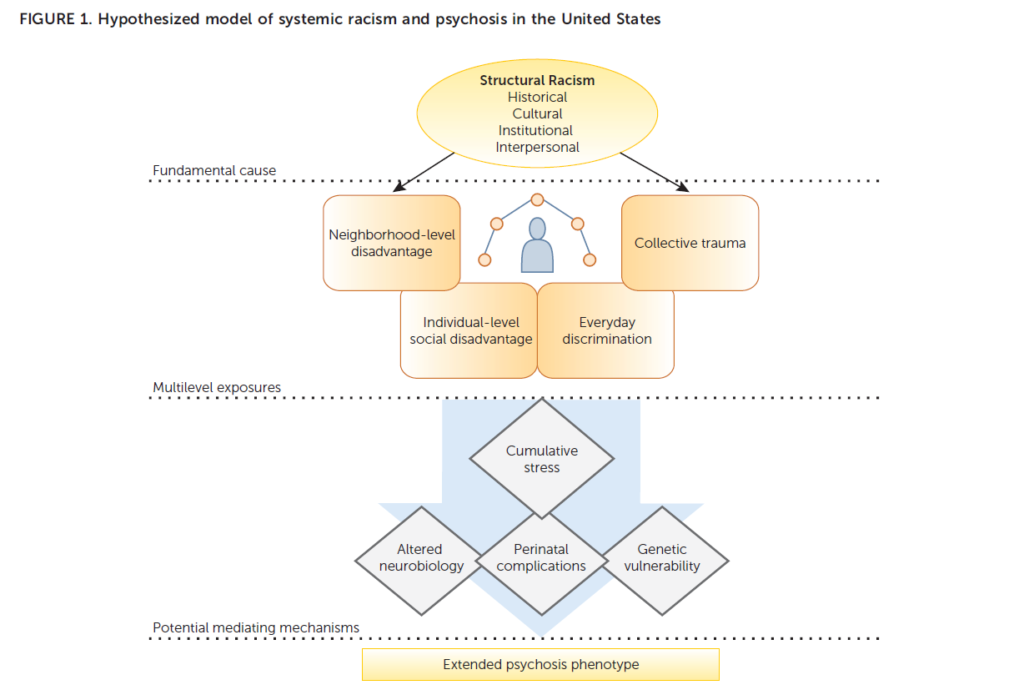
The model clearly points out that there are other factors in the development of psychosis (e.g., schizophrenia), but that the context of living with racism in every aspect of one’s life increases the odds that psychosis will occur. Clark et al. (1999) and Shelly Harrell (2000) also have much to offer on the relationship between the stress of coping with racism and mental health. Unfortunately, it is also the case that psychologists’ racial biases make it more likely that people of color will be misdiagnosed. In particular, patients of color are more likely than White patients to be diagnosed with a psychotic disorder when they actually present with symptoms of a mood disorder such as depression (Londoño Tobón et al., 2021).
White therapists who are unaware of their own racist assumptions and ideas often fail to work well with their clients of color, which is likely responsible, at least in part, for the fact that people of color underutilize mental health services and often end their therapy sessions too soon. Williams and Hastead (2019) offer White counselors some excellent recommendations on how to establish a solid, effective working relationship with their clients of color. Not only do we need more antiracist White therapists, we need more therapists of color, too, for those clients who prefer to work with someone who has a deep, personal understanding of the issues they face.

David Paul, a neurosurgery resident at the University of Rochester (and a former student of mine at Hope College, I have to say), has written a lovely, heartbreaking essay about the tragedies that can occur when Black people with mental health problems have an encounter with the police. It is a compelling reminder that racism is everywhere, all the time, and it makes everything worse for those who have to deal with it.
While you’re here, take a look at these specific suggestions for promoting justice in health and healthcare from The Othering & Belonging Institute at UC Berkeley. Just scroll down a bit along the outline in the left margin.
Do you want to know more? Spend 20 minutes with the remarkable David Williams and I will send you one college credit, affixed with my personal signature, suitable for framing and not much else. But you’ll know a lot more than you do now.
The Bottom Line: The racialized nature of our society, and the racism that justifies it, are stressful—often very stressful—and difficult to escape. The result is a wide assortment of problems with the physical and mental health of those who pay the price. We need to reduce both racialization and racism, but also improve health services for people of color.

